Guinea Bissau has abruptly halted a controversial hepatitis B vaccine study funded by the administration of US President Donald Trump, igniting a fierce debate about ethics, sovereignty, and the protection of newborn lives. The proposed trial, which aimed to enrol thousands of infants in a revised immunisation schedule, was stopped after the World Health Organization raised alarm over its design and potential consequences.
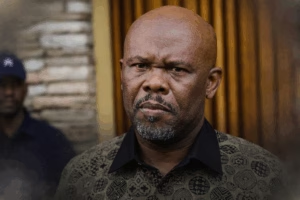
Foreign Minister Joao Bernardo Vieira delivered the government’s position with unmistakable clarity, shutting down speculation that the study might proceed under revised terms. In remarks carried internationally, he declared,
“It’s not going to happen, period.”
His statement signalled a decisive assertion of national authority, at a moment when public health policy and international collaboration have become increasingly sensitive in many African states.
Ethical Storm Over Infant Immunisation
At the centre of the controversy was the proposed enrolment of approximately 14,000 newborns in a hepatitis B trial financed by a 1.6 million dollar grant from the US Centers for Disease Control and Prevention. The study would have randomly assigned infants to receive the vaccine either at birth or at six weeks, a shift that researchers argued could yield valuable scientific insight.
Critics, however, warned that such randomisation would effectively deny half of the babies the birth dose, a move viewed by many public health authorities as unacceptable. The World Health Organization delivered a blunt assessment in an official statement, describing the trial as
“unethical”
and cautioning that withholding the vaccine could cause
“irreversible harm.”
The agency emphasised that the birth dose is
“an effective and essential public health intervention, with a proven record,”
noting that it prevents between 70 and 95 percent of cases of mother to child transmission.
Local Voices Demand Accountability
Domestic opposition to the trial had been building for months before the final decision. Former health minister Magda Robalo emerged as one of the most vocal critics, publicly challenging the scientific and ethical foundations of the project. Speaking to an international science journal, she argued that the proposal crossed a line in a country already grappling with fragile healthcare infrastructure.
Her position was unequivocal, stating,
“not acceptable and it should not go on.”
That criticism resonated within segments of Guinea Bissau’s medical community and civil society, where concerns about informed consent, oversight capacity, and the vulnerability of newborn participants were widely discussed. In a nation where trust in institutions can be fragile, the optics of a foreign funded experiment on infants carried profound political weight.
Science Or Politics
Researchers affiliated with the Bandim Health Project, operated by the University of Southern Denmark, defended the scientific rationale behind the study. Lead investigator Frederik Schaltz Buchholzer suggested that what began as a technical debate over vaccination timing had become entangled in political sensitivities. According to him, the discourse drifted away from empirical evidence toward broader narratives about external influence.
Supporters of the research contended that examining alternative vaccination schedules could generate data relevant not only to Guinea Bissau but to other high burden settings. Yet the trial had already faced turbulence earlier this year, when it was suspended pending an ethics review. Health officials revealed that the national committee responsible for oversight had not fully reviewed the protocol, raising procedural red flags before international criticism intensified.
African Sovereignty And Global Health
The controversy also revived longstanding questions about who controls medical research on the African continent. Africa Centers for Disease Control and Prevention Director General Jean Kaseya made it clear that African health authorities must retain command over studies conducted within their borders. His stance reflected a broader continental sentiment, shaped by historical experiences where research agendas were sometimes perceived as externally driven.
Guinea Bissau remains one of West Africa’s poorest countries, with hepatitis B rates among the highest globally. The government has pledged to introduce a birth dose of the vaccine into its national immunisation schedule by 2028, aligning with global public health recommendations. By cancelling the US funded trial, officials have signalled that while international partnerships remain important, ethical safeguards and national oversight will not be compromised when the health of newborn citizens is at stake.